◉ Results : A positive result is indicated by the presence of a bright pink color (fuchsia) in the agar slant. A negative result if no color change in the agar slant
☰ Content :
- Ⅰ. Overview
- Ⅱ. Principle
- Ⅲ. Procedure and results
- Ⅳ. Helicobacter pylori case
- Ⅴ. bacteria urease positive / negative
- Ⅵ. Limits and technical advice
Ⅰ. Overview
Urease test is used to identify bacteria capable of hydrolyzing urea using the enzyme urease. It is commonly used to distinguish the genus Proteus from other enteric bacteria.
Reoch, in 1875, proposed to test the alkaline fermentation of urea and the production of ammonia by bacteria to determine an organism's ability to produce urease, alkalinization causes a purplish-red coloration of the medium in presence of phenol red
- It can be used to detect the presence of Helicobacter pylori
- This test can also be used to differentiate between yeasts : Candida albicans (negative urease) and Cryptococcus neoformans (rapid production of urease).
Ⅱ. Principle
● Hydrolysis of urea by urease , a constitutively expressed enzyme, produces ammonia and CO2. The formation of ammonia alkalizes the medium and the change in pH is detected by the change in color from phenol red from light orange at pH 6.8 to magenta (pink) at pH 8.1.
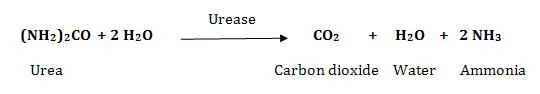
the reaction of the Urease test
Ⅲ. Procedure and results
◉ Two types of media are commonly used to detect urease activity :
1- Solid medium : Christensen Urea Agar Slant
- Strongly inoculate the slant (from a pure 18-24 hour culture) by streaking the agar surface in a zigzag fashion.
- Incubate inoculated tubes with loosened caps at 35-37 ° C for 24-48 hours
- Examine the slopes for color change after 6 hours and after overnight incubation. Longer periods may be necessary
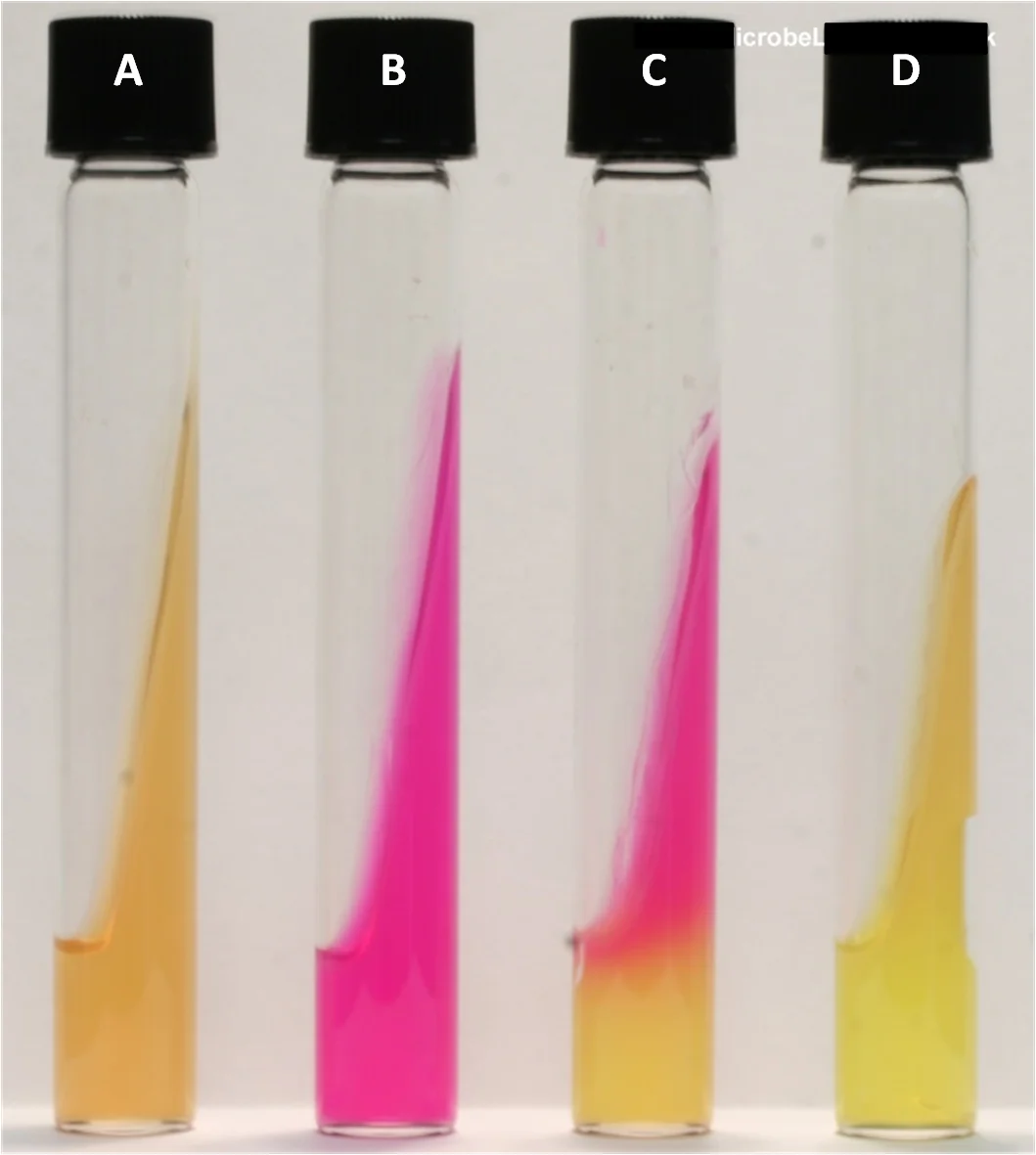
(A) unseeded, (B) Proteus mirabilis (rapid positive urease), (C) Klebsiella pneumoniae (delayed positive urease), (D) Escherichia coli (urease negative). (ASM MicrobeLibrery)
2- Liquid medium : Rustigian Stuart Urea Broth
- Inoculate the broth abundantly from a pure culture for 18 to 24 hours
- Gently swirl the tube to suspend the colonies
- Incubate inoculated tubes with loosened caps at 35 ° C in an incubator or water bath for 24-48 hours
- Examine broths for color change at 8, 12, 24 and 48 hour incubation
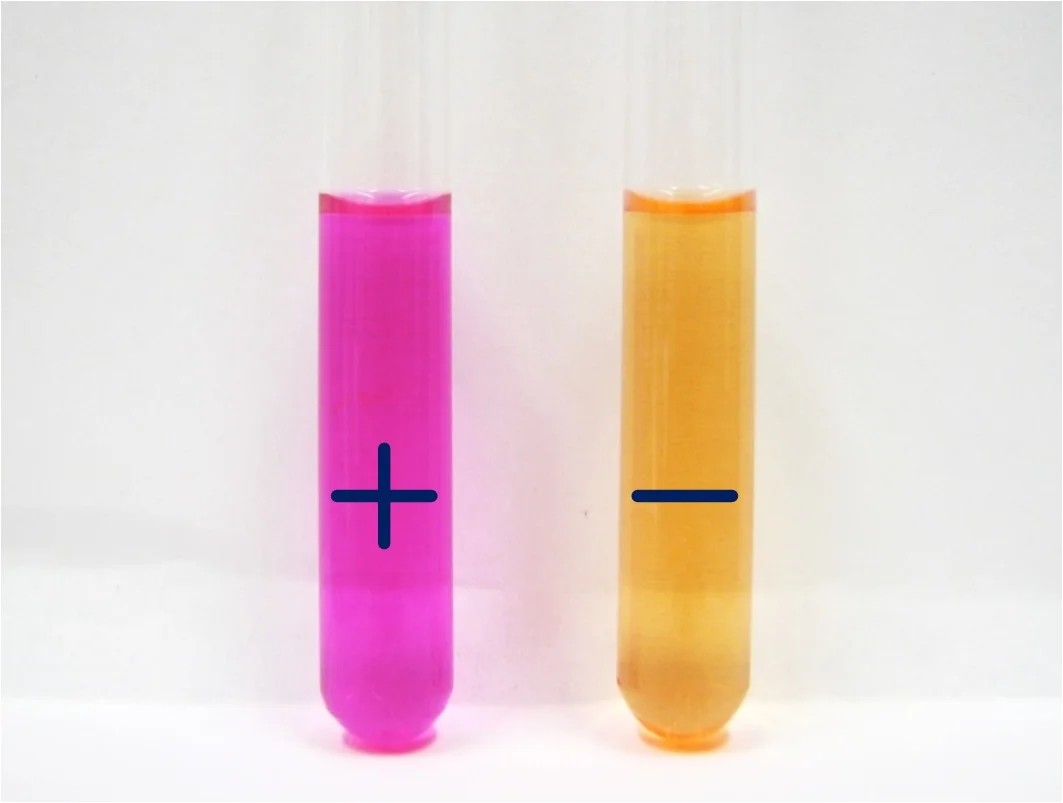
Urease test reaction results (source :ASM MicrobeLibrery)
◉ Results : A positive result is indicated by the presence of a bright pink color (fuchsia) in the broth. A negative result if no color change in the broth
Ⅳ- Helicobacter pylori case
Helicobacter pylori breaks up urea quickly, usually within 30 seconds. Its speed is a key distinguishing factor for H. pylori from other Helicobacter species.
Many special tests and media have been developed for the detection of H. pylori in the clinical laboratory.
1- Rapid urease test
The Urease Rapid Test , also known as the Campylobacter-like organism test (CLO) , is a rapid test for the diagnosis of Helicobacter pylori infection . The principle of the test is the ability of H. pylori to secrete the enzyme urease, the sample (eg gastric biopsy) is placed in a gel containing urea. The urease produced by H. pylori rapidly hydrolyzes urea, producing ammonia, which causes the indicator to change color.
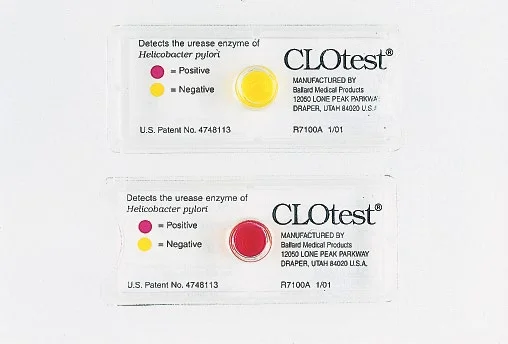
CLO test(Atlas of Bacteriology)
◉ Results : Results can be interpreted in 1 minute up to 3 hours, although the CLO test may be suspended for up to 24 hours in some cases
2- Urea breath test
The urea breath test is generally considered a simple, non-invasive, and accurate test to demonstrate Helicobacter pylori infection.
The principle of the test is simple. Orally administered urea, labeled isotopically with 14C or 13C (preferable choice), is hydrolyzed by the enzyme urease of H. pylori and the labeled CO2 is exhaled in the breath.
The labeled CO2 is detected either by a scintillation counter (Carbon-14) and isotope ratio mass spectrometry, or by mass correlation spectrometry (Carbon-13).
The main indication for UBT is confirmation of successful eradication with a sensitivity and specificity between 95 and 100%. To avoid false negative results, testing should be done 4-6 weeks after stopping treatment and 5 days after stopping antacids.
The test is also an ideal tool to check for infection when an ulcer is found on endoscopy, but biopsy samples cannot be taken due to the anticoagulant treatment.

Urea breath test
Ⅴ- Urease positive and negative test
◍ Positive and negative urease bacteria (9, 10, 11) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Bacteria | Urease positive | Variable urease | Negative urease | ||||||
| Enterobacteriaceae | Proteus , Klebsiella (lent) | / | Salmonella, Citrobacter, Escherichia coli, Edwardsiella, Shigella, Providencia, Enterobacter, Hafnia alvei, Serratia marcescens et liquefaciens | ||||||
| Yersinia spp. | Y.enterocolitica, Y.pseudotuberculosis | / | Y.pestis | ||||||
| Vibrionaceae | / | / | Aeromonas, Plesiomonas, Vibrio | ||||||
| Haemophilus influenzae | biotypes : I II III IV | / | biotypes : V VI VII VIII | ||||||
| Bordetella spp. | B. parapertussis(24 h), B. bronchiseptica(24 h) | / | B. pertussis, B. trematum, B. holmesii | ||||||
| Brucella spp. | B. suis , B. canis (fast) | B. melitensis B. abortus (plus long ou peut être négatif) | / | ||||||
| Bartonella spp. | / | / | Bartonella spp. | ||||||
| Helicobacter species | H. pylori, H. heilmannii | / | H. cinaedi, H. fennelliae | ||||||
| Ureaplasma urealyticum | Ureaplasma urealyticum | / | / | ||||||
| Streptococcus spp | S. vestibularis (Group Salivarius) | / | Group Mitis, Group Anginosus, Group Mutans | ||||||
Ⅵ- Limits and technical tips
- Urea broth is a highly buffered medium requiring large amounts of ammonia to raise the pH above 8.0, resulting in a color change.
- Urea media if exposed to light may develop peroxide, which may interfere with the urease test. Urea is also known to undergo self-hydrolysis; it is therefore advisable to store the media in the refrigerator at 4-8 ° C.
References:
- Public health England : Identification of Enterobacteriaceae
- Public health England : Urease test
- Biorad manuel : UREA INDOLE
- American society for microbiology : Urease Test Protocol
- ASM MicrobeLibrery
- M Peeters: a diagnostic tool in the management of Helicobacter pylori-related gastrointestinal diseases
- Senthilkumar Sankararaman; Leila Moosavi : Urea Breath Test
- Color Atlas of Medical Bacteriology (ASM Books) 3rd Edition