Summary :
◉ Définition
Serratia marcescens is an opportunistic bacterium, commonly found in the environment, responsible for nosocomial infections and epidemics, particularly in intensive care units.
It was discovered by Bizio, an Italian pharmacist, in 1819, when he identified it as a cause of the bloody discoloration of cornmeal porridge.
It is a Gram-negative bacillus that belongs to the Yersiniaceae family. It is characterized by its ability to produce a red pigment called prodigiosine.
Infections caused by Serratia marcescens can be difficult to treat due to their resistance to a variety of antibiotics.

◉ Epidemiology
Serratia thrives in moist environments, it is found in soil, water, plants, animals and the human intestine. In hospital settings, it frequently colonizes medical devices , such as bronchoscopes, urinary catheters and water supplies, while long-term carry in the hands of healthcare workers has also been reported.
The predominant mode of spread of S. marcescens is hand-to-hand transmission by hospital staff.
A person colonized with Serratia can become infected due to invasive devices, surgery, and the severity of an underlying disease.
◉ Clinical Manifestations
S. marcescens is considered an opportunistic pathogen, which means that it only causes infections under certain conditions, such as a weakened immune system.
However, bacteria can be involved in various clinical pictures, it is associated with urinary tract infections, endocarditis, osteomyelitis, sepsis, wound infections, meningitis and especially eye and respiratory infections.
- Ocular involvement: Serratia can invade human corneal epithelial cells and cause keratitis (particularly contact lens related), conjunctivitis, endophthalmitis or ulcers corneal.
- Infections of the surgical site, skin and soft tissues.
- Central nervous system damage: following lumbar puncture, spinal injections or other surgeries.
- Joint involvement: septic arthritis following diagnostic and therapeutic intra-articular injections.
- Endocarditis: This is rarely a cause of infective endocarditis (more common in drug addicts), but in cases of endocarditis it follows a rapid and devastating course.
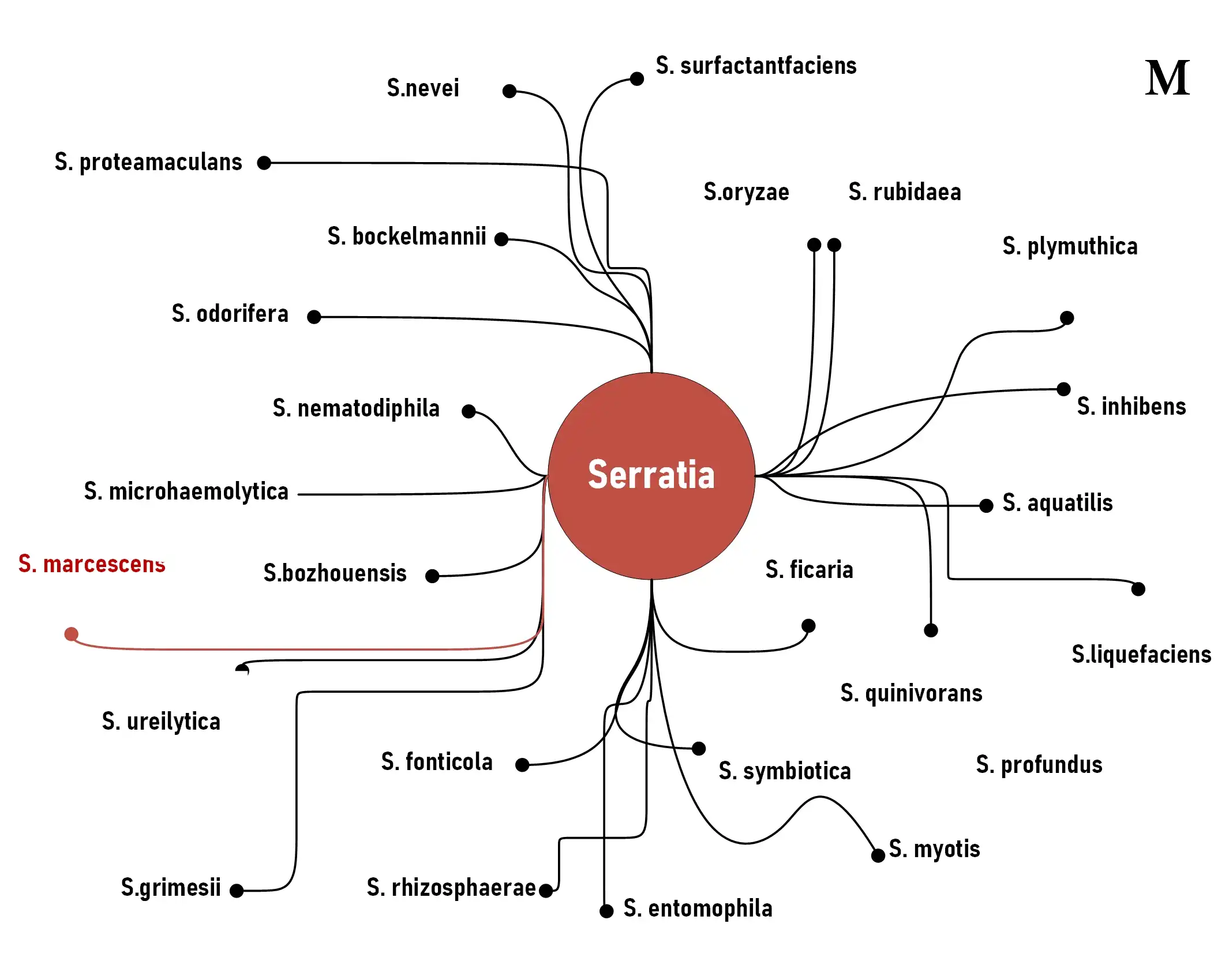
◉ Classification and Nomenclature
According to NCBI Taxonomy Browser, The genus Serratia, which is part of the order Enterobacterales and the family Yersiniaceae, comprises more than 20 species, eight of which are known for causing infections in humans.
S. marcescens is the main human pathogen of the genus, it was named in honor of the Italian physicist Serratia who invented the steamer and marcescens, which is the Latin word for "decompose", because the bloody discoloration on the cornmeal disappeared quickly.
◉ Bacteriological Characters and Identification
Serratia is a Gram-negative bacillus that is about 3-6 μm long and up to 1 μm wide. These bacteria can easily grow on routine microbiological culture media (BHIB, trypticase soy, nutrient agars).
Some Serratia spp. are pigmented, including S.rubidaea, S.plymuthica and some strains of S. marcescens, produce a red pigment called prodigiosine.
- Among the characters that helps you identify Serratia marcescens :
- Motility : swimming (motility in a liquid environment) and swarming (motility on a solid surface).
- ONPG: positive
- It ferments glucose, maltose, mannitol, trehalose and sucrose.
- Lactose: no fermentation or slow fermentation.
- Gas production: negative
- H2S : negative
- Indole test : negative
- VP (Voges-Proskauer) test : positive
- Methyl red : negative.
- LDC and ODC : positive
- TDA : negative
- Urea hydrolysis(Urease) : negative
- Production of enzymes: DNAse, lipase and gelatinase.
- Catalase test : positive
- Oxidase test: negative
- Citrate test : positive
- On TSI agar, Serratia can be a slow fermenter of lactose, causing an alkaline reaction in the slant (tube with yellow butt and red slant).
- On MacConkey agar, it grows well after incubation aerobically at 35°C for 18 to 24 h.
- On Hecktoen agar, it is salmon-colored due to the fermentation of sucrose.
- On Mueller-Hinton agar, it presents a cocarde growth around polymyxin B disks
- DNA toluidine blue agar may be required for isolation of Serratia from non-sterile sources.
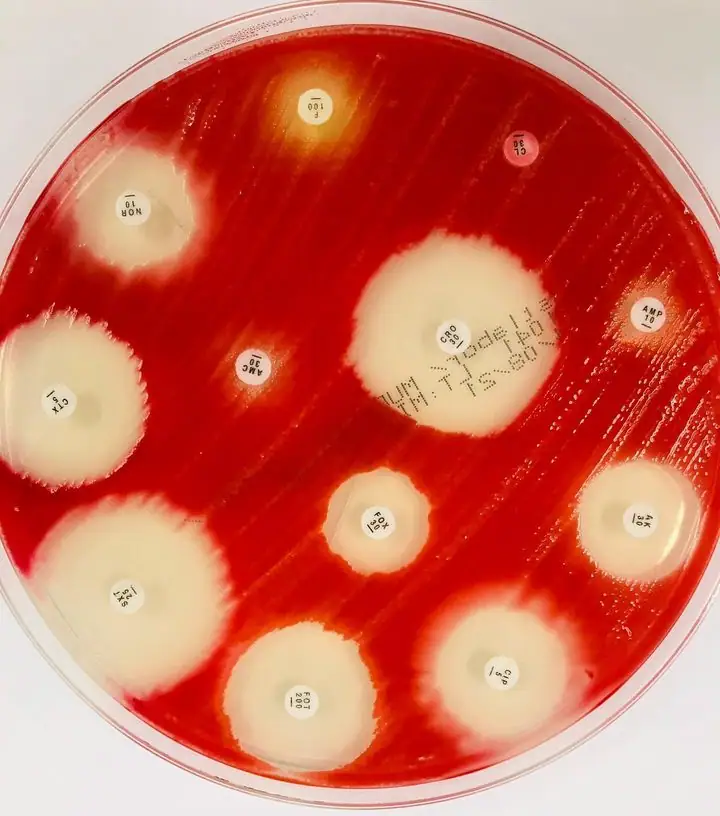
◉ Resistance
S. marcescens is resistant to a wide range of antibiotics, including penicillins and narrow-spectrum cephalosporins, cefuroxime, cephamycins, macrolides, tetracycline, nitrofurantoin and colistin.
◉ Surveillance
Patients with Serratia infections should be monitored for clinical response during treatment.
In cases where the patient does not improve clinically on cephalosporin therapy, the emergence of derepressed AmpC mutants may be the cause. Hence the interest in repeating the sensitivity tests and adjusting the treatment.