Content :
Experiencing a vaginal yeast infection is a relatively common condition that can be quite uncomfortable, characterized by symptoms such as persistent itching and abnormal discharge. In this article, we explain the causes of vaginal candidiasis, its symptoms, diagnosis and possible treatments.
◉ Having Vaginal Yeast Infection
Vaginal yeast infection , also referred to as vaginal candidiasis or vaginal mycosis, is a prevalent fungal infection among women. It is caused by an overgrowth of Candida fungi, particularly Candida albicans, in the vaginal area.
According to CDC, vaginal candida infections are quite common. In their lifetime, around 75% of all women are likely to experience at least one such infection, and up to 45% may have two or more.
Typical symptoms encompass itching, a burning sensation, redness, and swelling in the vaginal area, often accompanied by a thick, white discharge that resembles cottage cheese.
Despite its resemblance to sexually transmitted infections, vaginal mycosis is not categorized as one. Instead, it is often triggered by factors like hormonal fluctuations, antibiotic usage, a compromised immune system, diabetes, or vaginal irritation.
Treatment mainly revolves around antifungal medications, including creams, suppositories, or oral tablets.
◉ Is Vaginal Yeast Infection Contagious?
Although a vaginal yeast infection is not considered a sexually transmitted infection (STI), there is still a possibility of transmitting a yeast infection to a partner. Most doctors do not recommend having sex until the infection has cleared up.
Also, engaging in sexual activity while experiencing a yeast infection can potentially prolong the duration of the infection.
◉ 10 Causes and Risk Factors for Vaginal Yeast Infection
Vaginal yeast infection is primarily caused by the overgrowth of a fungus called Candida, specifically Candida albicans.
1. Candida overgrowth
Candida is a fungus that normally exists in the vagina along with other microorganisms. However, certain circumstances can disrupt the balance of the vaginal flora, resulting in an overgrowth of Candida.
2. Weakened immune system
Individuals with weakened immune systems, such as those with HIV/AIDS or undergoing chemotherapy, are more susceptible to vaginal mycosis
3. Hormonal changes
Fluctuations in hormonal levels, particularly estrogen, can create an environment that favors the growth of Candida. This is why vaginal mycosis is more common during pregnancy, menopause, or while taking hormonal contraceptives.
4. Antibiotic use
Antibiotics can disrupt the natural balance of microorganisms in the vagina by killing off the beneficial bacteria that help control Candida. This disruption allows an overgrowth of Candida to occur.
5. Use of Corticosteroids
Prolonged use of corticosteroid medications (such as prednisone), can lead to the development of a yeast infection or worsen an existing one..
6. Diabetes
Individuals with poorly controlled or uncontrolled diabetes tend to have elevated sugar levels in both their blood and vaginal secretions. Candida, being nourished by sugar, can thrive and grow in such environments with higher glucose levels.
7. Sexual transmission
Although uncommon, vaginal mycosis can be transmitted through sexual intercourse, particularly if one partner has an active infection. However, it is not considered a sexually transmitted infection (STI) as it can occur in individuals who have never had sexual intercourse.
8. Irritant Factors
Using overly aggressive personal hygiene products, employing abrasive cleaning methods, frequently engaging in vaginal douching can all elevate the risk of developing a fungal infection.
9. Tight Clothing
Wearing synthetic, non-breathable fabrics and tight clothing can create a warm, moist environment ideal for yeast growth.
10. Sex with multiple partners
Having multiple sexual partners might also increase the chances of coming into contact with someone who has a yeast infection.
Note: While certain factors can contribute to vaginal yeast infections, the exact cause can vary among individuals, and recurring infections might result from a combination of these factors.
◉ Signs and Symptoms
Vaginal yeast infection symptoms can vary in intensity from mild to severe. Some common signs of a vaginal yeast infection include:
- Vaginal itching and irritation: The itchiness may be severe and can cause significant discomfort.
- Thick, white, and clumpy vaginal discharge: The discharge is typically thick and white, resembling cottage cheese.
- Odor: An unusual odor, often described as yeasty or similar to bread, can be present in some cases.
- Burning sensation during urination: Irritation from the infection can cause discomfort (dysuria) or a burning sensation when urinating.
- Redness and swelling: The vaginal tissues may appear red, swollen, and inflamed due to the infection.
- Soreness and discomfort during sexual intercourse: The infection can cause pain and discomfort during sexual intercourse.
- Rash or redness around the vulva: Some individuals may develop a rash or redness around the vulva and outer vagina.
Note: If you suspect a vaginal yeast infection or experience persistent symptoms, seeking medical attention for an accurate diagnosis and appropriate treatment is advisable.
◉ Diagnosis
Vaginal yeast infection can be diagnosed based on symptoms, physical examination, and laboratory tests. Most commonly, a healthcare provider may diagnose vaginal mycosis based on the following:
◉ Reviewing Medical History
Healthcare professionals inquire about your medical history, which helps in understanding potential risk factors and prior occurrences of yeast infections.
◉ Symptom Assessment
The presence of common symptoms such as itching, burning, redness, swelling, and abnormal discharge (usually thick, white, and odorless) in the vaginal area.
◉ Conducting a Gynecological Examination
A visual examination of the vagina and surrounding area to check for signs of infection, including swelling, redness, and discharge.
◉ Laboratory tests
To confirm the diagnosis, laboratory tests are employed. A vaginal swab or discharge sample is collected and sent for testing. These tests help identify the presence of yeast and confirm the infection.
- Microscopic Examination: A sample of vaginal discharge is examined under a microscope, wet mount or after staining, to detect the presence of yeast cells, clue cells (indicative of bacterial vaginosis ), and other types of cells.
- Cultures: Vaginal swabs or samples are cultured on specific media, such as Sabouraud dextrose agar, to facilitate the growth of fungi and inhibit other species. It generally requires several days of incubation.
- PCR (Polymerase Chain Reaction): It's a sensitive method that can identify the presence of yeast by amplifying their genetic material.
- pH testing: can only determine if your vaginal pH is within the normal range. It can provide an indication of a potential infection but not confirm it definitively.
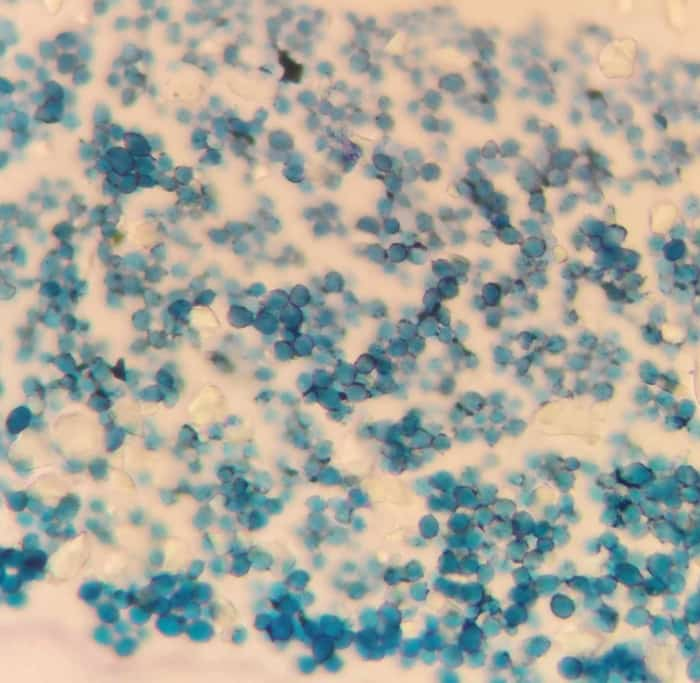
Yeast Infection Under Microscope
◉ Treatment
The treatment for vaginal mycosis typically involves antifungal medications. These medications can be administered orally, such as fluconazole, or applied topically in the form of creams, ointments, or suppositories that contain antifungal agents like clotrimazole, miconazole, or terconazole.
In addition to medication, there are several self-care measures that can be taken to help manage and prevent vaginal yeast infection:
- Good hygiene practices: genital area must be kept clean & dry. Don't use douches or scented products in vaginal area, as they can disrupt the natural balance of healthy bacteria.
- Loose-fitting clothing: Wear breathable cotton underwear and avoid tight-fitting pants or synthetic fabrics that trap moisture.
- Avoid irritants: Steer clear of irritants such as chemical-laden feminine hygiene products, strong detergents, or fabric softeners that may cause irritation and contribute to vaginal mycosis.
- Limit sugar intake: Reducing the consumption of sugary foods and beverages may help prevent or manage yeast infections, as yeast thrives on sugar.
- Probiotic supplements: Some studies suggest that taking probiotics can help to maintain a healthy vaginal balance by promoting the growth of beneficial bacteria. Probiotics can be found in supplement form or in certain foods like yogurt.
It is important to finish the entire course of medication prescribed by the healthcare provider, even if symptoms improve before completing the treatment.
If symptoms persist or worsen despite treatment, consulting with a healthcare provider is recommended as there could be other underlying causes.
◉ Conclusion
Yeast Vaginal Infections are common and result from Candida overgrowth. Diagnosis involves considering symptoms, history, exams, and tests. Early detection and proper management are key to maintaining vaginal health.