Content:
◉ Introduction
Enterococcus faecalis is a type of bacteria that normally lives in the human gastrointestinal tract as a normal flora, and can also be found in the oral cavity and vaginal tract, but can cause infections in other parts of the body, especially in hospital settings.
Some of the common infections caused by E. faecalis are urinary tract infections, wound infections, blood infections, and heart inflammation.
To diagnose an E. faecalis infection, a sample of urine, blood or other fluid is taken and cultured to identify the bacteria and its sensitivity to antibiotics.
◉ Classification and Nomenclature
Enterococcus faecalis belongs to the genus Enterococcus, in the family Enterococcaceae, order Lactobacillales, and class Bacilli.
- The name Enterococcus means intestinal coccal, reflecting their common habitat.
- It is called "faecalis" because it was first isolated from human fecal samples.
E. faecalis was first isolated and identified in 1899 by the German microbiologist Fritz Schmalz. It was initially classified as Streptococcus faecalis due to its similarities with other streptococci.
In 1984, based on biochemical, genetic, and cell wall characteristics, the International Committee on Systematics of Prokaryotes proposed reclassifying the group Streptococcus faecalis into a distinct genus, Enterococcus.
◉ Epidemiology
Enterococci are commonly found in the human and animal digestive tract, often colonizing the skin and genitourinary pathways. Enterococcus faecalis is the predominant species within the genus, constituting 80 to 90% of clinical isolates.
These bacteria are opportunistic and ubiquitous, capable of surviving for several weeks in the hospital environment, especially on contaminated surfaces and laundry.
Despite being relatively low in virulence factors compared to other bacteria, the accumulation of resistance mechanisms and the increasing frequency of their isolation, particularly in nosocomial infections, have sparked renewed interest in this bacterial genus.
Infections with Enterococcus faecalis are more common in individuals with weakened immune systems, those suffering from chronic diseases, cancer, organ transplants, or invasive procedures. Elderly individuals, infants, and pregnant women are also more susceptible to E. faecalis infections.
Enterococci faecalis are transmitted through direct contact, via surfaces (able to survive up to 4 months on dry surfaces), as well as through water and contaminated food.
◉ Clinical Manifestations
The symptoms of an Enterococcus faecalis infection depend on the location and severity of the infection, as well as the person's immune status and underlying health conditions.
Some of the common clinical manifestations of E. faecalis infections are:
◉ 1- Urinary tract infections (UTIs)
Urinary infection by Enterococcus faecalis is more common in hospital settings, particularly if the patient is male, catheterized, or has received broad-spectrum antibiotic therapy.
The infection can be monobacterial or associated with other germs (Gram-negative bacteria), causing either colonization, asymptomatic bacteriuria, or typical urinary infections (pain, burning when urinating, polyuria, cloudy or bloody urine, etc.).
◉ 2- Endocarditis
This is an infection of the inner lining of the heart or heart valves. Enterococcus faecalis can cause endocarditis by entering the bloodstream through the digestive or genitourinary tract, during dental procedures, intravenous drug use, or other means.
Endocarditis is more common as the patient gets older or if there is pre-existing heart disease. It can cause fever, chills, fatigue, chest pain, shortness of breath, and a heart murmur.
◉ 3- Bacteremia
Enterococcus faecalis can cause bacteremia by contaminating a catheter, a dialysis port or spreading from a urinary, biliary, intra-abdominal or superficial site (the skin of a burn victim).
Bacteremias are often nosocomial with a severe prognosis, it can cause fever, chills, fatigue, headaches, rapid breathing and low blood pressure or even death.
◉ 4- Wound infections
They typically occur as a result of contamination of a wound, either through direct contact with the bacterium or from its spread from another infected site with Enterococcus faecalis.
These infections can manifest with symptoms such as localized pain, swelling, redness, and discharge. In more severe cases, systemic symptoms like fever, chills, and fatigue may also be present.
◉ 5- Meningitis
E. faecalis can cause meningitis by entering the bloodstream through a head injury, surgery, or other means. Meningitis can cause fever, headache, stiff neck, sensitivity to light, confusion, and seizures.
◉ Identification and Bacteriological Characters
Enterococcus faecalis can be identified by its cultural, biochemical, and molecular characteristics. Some of the methods used for identification include:
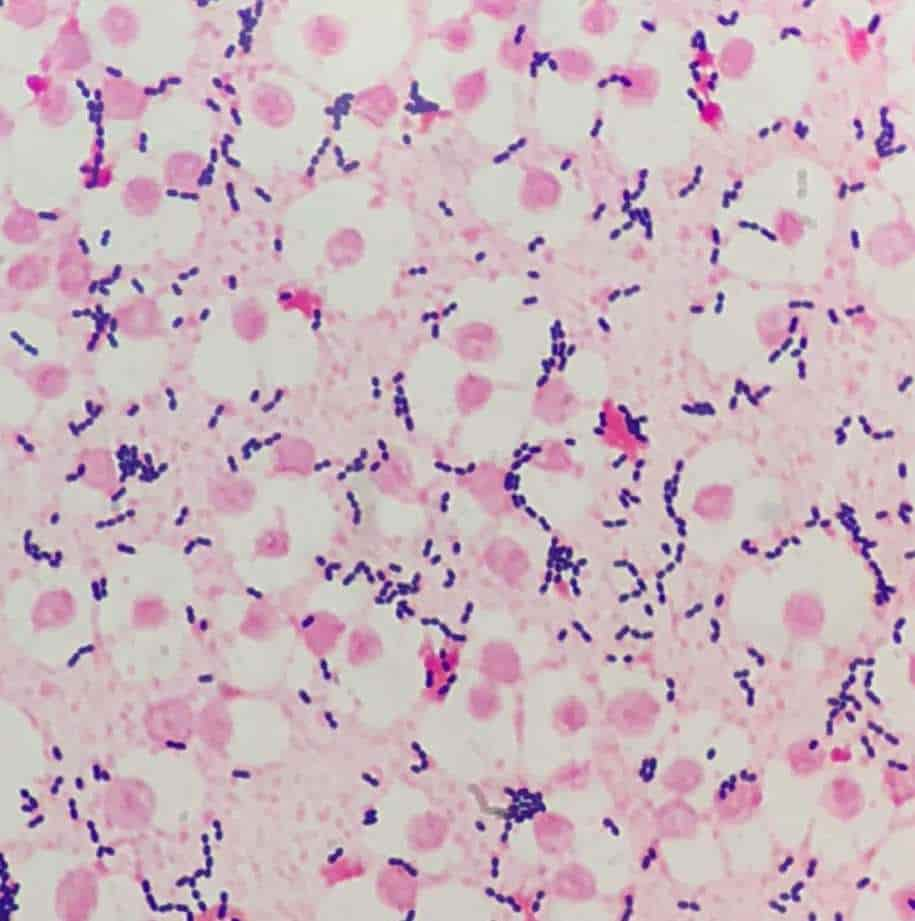
◉ 1- Direct examination
Under the microscope and after Gram staining, Enterococcus faecalis appears as oval or round Gram-positive cocci grouped in pairs or short chains.
◉ 2- Culture
Enterococcus faecalis grows easily on common culture media under normal atmospheric conditions, typically within 18 to 24 hours, at temperatures ranging from 10 to 45 °C.
E. faecalis produces small colonies (pinpoint colonies), smooth, gray, or whitish-gray in appearance, showing non-hemolytic (γ-hemolytic) characteristics, although some strains may be beta-hemolytic on blood agar.
They can also thrive in extreme conditions such as the presence of 6.5% NaCl, 40% bile salts, and at a pH of 9.5. These conditions are often used as diagnostic aids.
Bile-esculin-azide agar and CNA agar (Colistin Nalidixic Acid agar) are specific culture media that promote the growth of enterococci while inhibiting the growth of other bacteria.
◉ 3- Identification of the genus Enterococcus
- Oxidase test negative.
- Catalase test negative: This distinguishes it from catalase-positive genera like Staphylococcus and Micrococcus.
- PYR test positive : Most species of the genus Enterococcus produce pyrrolidonylarylamidase (PYR A).
- Growth on bile-esculin agar with esculin hydrolysis.
- Detection of Antigen D: Enterococci possess the Lancefield Group D antigen, linked to lipoteichoic acids in the cell wall. However, its demonstration is inconsistent and no longer of interest for identification purposes.
◉ 4- Identification of the Enterococcus faecalis species and biochemical characterization
Identifying the species of enterococci isolated from severe infections is crucial for effective treatment and epidemiological monitoring.
Resistance to potassium tellurite is a key characteristic for the rapid identification of Enterococcus faecalis. Additionally, E. faecalis is characterized by the following:
- Mobility: Generally non-motile.
- Yellow Pigment: Negative (-).
- Arginine Hydrolysis: Positive (+).
- Mannitol Utilization: Positive (+).
- Sorbitol Utilization: Positive (+).
- Raffinose Utilization: Positive (+).
- Sucrose Utilization: Positive (+).
- Sorbose Utilization: Negative (-).
- Voges-Proskauer (VP) test: Positive (+).
For more complete biochemical identification, biochemical galleries such as Api 20 strep or bacteriological identification automates (MicroScan WalkAway plus System, ALFRED 60/AST.. ) can be used.
◉ 5- Molecular diagnosis
E. faecalis can be identified by using polymerase chain reaction (PCR) to amplify specific genes.
◉ 6- Antibiotic resistance profile
The antibiotic resistance profile can also help differentiate between different species of enterococci:
- Enterococcus faecium species are resistant to ampicillin and highly resistant to imipenem.
- Enterococcus faecalis species are naturally resistant to lincosamides and streptogramin A and sensitive to imipenem.
- E. gallinarum and E. casseliflavus species have MICs of 4 to 32 mg/l for vancomycin.
◉ Resistance
Enterococcus faecalis is known for its ability to resist many antibiotics, making it harder to treat. This bacterium has the capability to form biofilms, which are bacterial communities adhering to surfaces and shielded by a matrix of extracellular substances.
The biofilm formation serves as protection against host immune responses, rendering Enterococcus faecalis even more resilient to antibiotics and disinfectants.
◉ Intrinsic resistance
Enterococcus faecalis is known for its intrinsic resistance to certain antibiotics, including oxacillin, penicillins, cephalosporins, monobactams, lincosamides, and streptogramin A (LSA phenotype). Additionally, it exhibits a low susceptibility to aminoglycosides due to the inefficient transport of these antibiotics across the cytoplasmic membrane.
◉ Acquired resistance
Enterococcus faecalis can acquire resistance to antibiotics by various mechanisms: production of penicillinase, increased expression of low affinity PLP5, alteration of the molecular target (resistance to streptomycin), acquisition of Van genes (A, B, D ,E,G). The latter are responsible for resistance at variable levels to vancomycin and teicoplanin.
◉ Surveillance
Surveillance of Enterococcus faecalis is important to monitor the prevalence, incidence, and resistance profiles of this bacterium, which can cause infections in various parts of the body, especially in hospitalized patients.
Surveillance methods include laboratory testing, reporting and tracking of enterococcal isolates, and infection control measures, such as hand hygiene, environmental cleaning, and appropriate use of antibiotics.
◉ Conclusion
In conclusion, Enterococcus faecalis is a bacterium that demands attention and further investigation. By enhancing our knowledge and implementing comprehensive strategies, we can better combat the challenges posed by this pathogen and improve patient outcomes in healthcare settings.