Content :
◉ Introduction
The direct Coombs test (DBT), also called the direct antiglobulin test (DAT), is a laboratory blood test used to detect the presence of Antibodies bound to the surface of red blood cells, which can lead to their destruction (hemolysis).
Invented in 1945 by scientist Robert Coombs, this test has since become an important tool for diagnosing certain anemias, blood infections and other diseases associated with damage to red blood cells.
The direct Coombs test is relatively simple to perform, but its interpretation can sometimes be difficult. It requires consideration of symptoms, patient medical history, test limits, and other medical test results to reach an accurate conclusion.

◉ Indications
The main indications of the direct Coombs test are as follows:
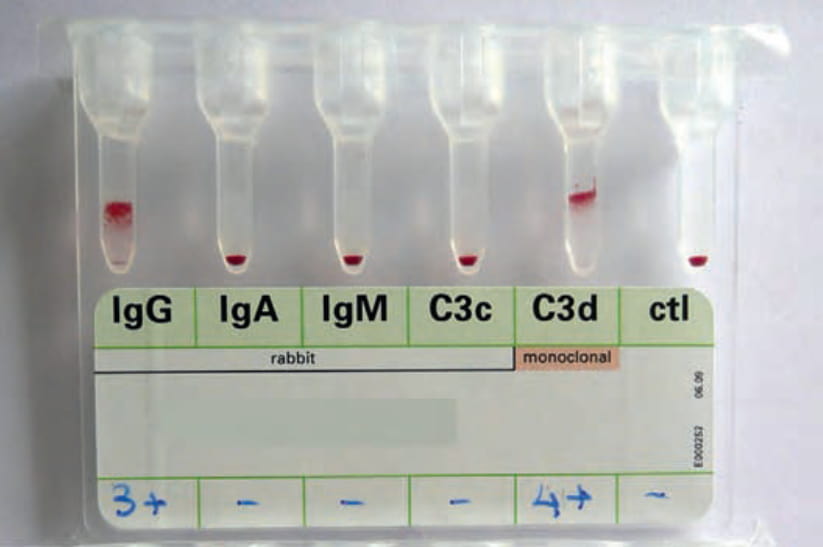
- Autoimmune hemolytic anemias (AIHA): represent the main indication for the direct Coombs test, where it is positive in 90% of AIHA cases. This test detects autoantibodies attached to the patient's red blood cells. The use of monospecific Coombs reagents can also help differentiate between warm antibody hemolytic anemia (IgG+ and C3+) and cold antibody hemolytic anemia (IgG- and C3+).
- Hemolytic disease of the newborn (HDN): It makes it possible to detect whether the recipient has antibodies directed against the antigens present on the transfused red blood cells, or whether antibodies are formed in response to the transfusion.
- Transfusion accidents: It allows the detection of the recipient's antibodies present on the recipient's red blood cells.
- Diagnosis of drug-induced immune hemolytic anemia.
◉ Principle
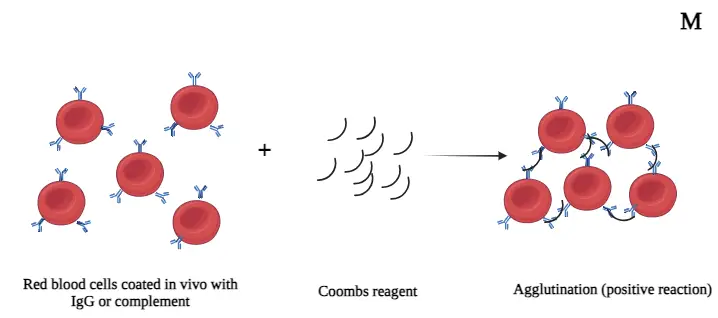
Normal human red blood cells can become sensitized in the presence of antibodies to an antigen they possess, but they will not clump together due to the specific nature of the antigen and antibody involved.
The direct antiglobulin test detects erythrocytes that have been sensitized by antibodies (igG) and/or complement (C3d) in vivo, i.e. in the patient's body.
The direct Coombs test is based on the principle of agglutination. When red blood cells are coated with antibodies, complement fragments, or both, the addition of anti-human globulin (AHG, also called Coombs reagent) causes agglutination. Unsensitized cells will not clump together.
◉ Equipment needed
Required materials include:
- EDTA: EDTA is the preferred type of anticoagulant for the test. It chelates Ca++ and Mg++ ions preventing in vitro binding of complement to red blood cells which can be mediated by naturally present antibodies
- 0.9% NaCl saline solution: Used for washing red blood cells.
- General laboratory equipment: Includes test tubes, pipettes, centrifuge, among other equipment needed to perform the test.
- Coombs reagent: Also known as Coombs antiglobulin or antihuman globulin. It is used to detect the presence of antibodies bound to red blood cells in the test.
- Positive control cells (IgG coated): Used to validate the test reaction and ensure its reliability.
The test can also be done with a gel in a tube, which is more convenient and more sensitive.
◉ Coombs reagent
The Coombs reagent, also known as Antihuman globulin (AHG), is produced by immunizing animals, usually rabbits, with globulin purified human. The animals then produce antibodies against human immunoglobulins and components of the complement system.
Before use, AHG is purified to remove contaminants. It is then used in direct Coombs tests and indirect to detect antibodies attached to red blood cells.
AHG reagents can be:
- Polyspecific, containing antibodies against both immunoglobulin G (IgG) and complement components (C3d).
- Monospecific, containing a single component, such as an anti-IgG or anti-C3d antibody.
AHG reagents specific for IgA or IgM or other complement fractions are not commonly available in most clinical laboratories, but can be used in reference laboratories for screening of difficult cases to diagnose.
◉ Procedure
Here is a general procedure for performing a direct Coombs test:
- Collect a blood sample from the patient in a tube containing EDTA.
- Centrifuge the tube to separate the plasma from the red blood cells.
- Wash the red blood cells three times with isotonic saline to remove contaminants.
- After the last wash, completely decant the supernatant.
- Collect 50 microliters of cell suspension from the patient into a new test tube.
- Add 2 drops of Anti-Human Globulin (AHG) to the patient's cell suspension in the test tube.
- Mix thoroughly and centrifuge the mixture at a speed of 1,500 rpm for 1 minute.
- Shake the tube gently and examine with the naked eye and under a microscope for agglutination.
- If agglutination is observed, the result is considered positive, indicating the presence of antibodies on the red blood cells.
If the test result is negative, to validate the result, add a drop of control cells (positive control), mix well and centrifuge the mixture at 1,500 rpm for 1 minute and look for agglutination. If no agglutination is observed, the result is invalid.
In practice, we start by using the polyspecific reagent capable of detecting both IgG and C3; then, in the event of a positive result, a monospecific test is subsequently carried out to characterize the antibody more precisely.
◉ Direct Coombs test Positive
The direct Coombs test can be positive in the following situations:
- Autoimmune hemolytic anemia (AIHA): In AIHA, antibodies produced by the immune system attack the body's own red blood cells, leading to their destruction and anemia.
- Hemolytic disease of the fetus and newborn (HFND): maternal antibodies attack the red blood cells of the fetus.
- Post-transfusion immune reaction: A positive direct Coombs test may occur after a blood transfusion if the recipient develops an immune reaction against the antigens present on the donor's red blood cells.
- Drug-induced hemolytic anemia.
- Patients with chronic lymphocytic leukemia (CLL), although this is not the case for all patients.
- Certain infections: Mycoplasma, HIV.
- There are cases where erythrocyte clumping can be seen in older people without the presence of known diseases that can cause clumping. In addition, certain medications can influence the formation of erythrocyte agglutinates.
◉ Direct Coombs test Negative
A negative direct Coombs test means that no antibodies or complement have been detected on the surface of the red blood cells by the Coombs reagents.
In some cases, even in the presence of autoimmune-mediated hemolysis, the antiglobulin test result may be negative. This is known as Coombs negative autoimmune hemolytic anemia.
If autoimmune hemolytic anemia is suspected despite a negative result on the direct Coombs test, more sensitive quantitative tests are needed to assess the amount of IgG on red blood cells.
◉ Conclusion
In summary, the direct Coombs test can be positive in various situations such as autoimmune hemolytic anemia or post-transfusion immune reactions. However, a negative result cannot completely rule out these conditions. Accurate interpretation requires a thorough assessment of the patient's symptoms and medical history.