Content:
◉ Introduction
Malaria is a potentially fatal but also treatable and preventable disease transmitted to humans through the bites of female Anopheles mosquitoes. The disease is more prevalent in tropical countries.
A malarial infection is caused by a parasite called Plasmodium, carried by the mosquitoes mentioned previously.
Symptoms vary from patient to patient, ranging from mild such as fever and chills, moderate such as headache and fatigue, to severe such as confusion, seizures and difficulty breathing. .
Serious infections often occur in patients with weakened immune systems, in infants and children under 5 years of age, as well as in pregnant women and travelers.
◉ Pathophysiology
Malaria disease is caused by a single-celled parasite of the genus Plasmodium, mainly transmitted by the bite of a female Anopheles mosquito.
Malaria transmission cycle
- An uninfected mosquito feeds on the blood of an infected person, thereby becoming infected with the parasite itself.
- When this infected mosquito bites an uninfected person, it transmits the malaria parasites, thus leading to their infection.
- The parasites then enter the infected person's liver, where some types can remain dormant for a long time, sometimes up to a year.
- After maturation in the liver, the parasites enter the bloodstream and infect red blood cells. It is at this stage that symptoms of malaria usually manifest in patients.
- If an uninfected mosquito bites a person at this stage of the cycle, it in turn becomes infected and can transmit malaria to other people during subsequent bites.
Malaria transmission cycle
Other modes of malaria transmission are also observed, since the Plasmodium parasites, responsible for this disease, target red blood cells. Thus, individuals can contract malaria following exposure to infected blood, in particular by:
- Transplacental transmission, where the parasite can be passed from mother to fetus.
- Blood transfusions, when a transfusion is carried out with contaminated blood.
- Sharing of needles, usually seen when used for injecting drugs.
◉ Malaria species
Malaria is caused by four species of parasites of the genus Plasmodium: P. vivax, P. ovale, P. malariae and P. falciparum. Among these, P. vivax and P. falciparum infections are the most prevalent worldwide./p>
◉ Symptoms and signs of malaria
The clinical presentation of malaria is variable and can include a range of symptoms and signs:
- Fever: Fever is the main symptom of malaria. It rises slowly and persists for seven days or more.
- Headaches and muscle pain.
- Discomfort and weakness.
- Gastrointestinal disorders: nausea, vomiting and diarrhea.
- Shivers: tremors occurring throughout the body.
- Respiratory symptoms: chest pain, difficulty breathing and cough.
- Jaundice: a yellowish discoloration of the skin and mucous membranes.
- Convulsions.
- Confusion.
- Dark urine.
Children are more likely to have nonspecific symptoms such as lethargy, malaise, nausea, abdominal cramps and excessive sleeping (drowsiness). Additionally, children are more likely to develop hepatosplenomegaly and severe anemia without major organ dysfunction than adults.
In severe malaria, patients generally present with more seizures than other symptoms, as well as concomitant hypoglycemia and sepsis.
◉ Malaria Diagnosis
Medical history
For an accurate diagnosis, the doctor must take a complete history of the patient, including:
- Place of Residence: Identify the patient's place of residence, particularly if they reside in an area where malaria is endemic.
- Recent Travel: Investigate the patient's recent travel to areas where malaria is common.
- Taking Chemoprophylaxis: Ask if the patient has taken malaria chemoprophylaxis medications.
- Contact with Sick People: Find out about any recent contact with people suffering from malaria.
- Exposure to Insects and Arthropods: Ask about any recent exposure to mosquitoes and other insects.
- Contact with Animals: Investigate contact with domestic, farm and wild animals.
Additionally, the doctor should ask for a history of:
- Anemia: History of anemia or low hemoglobin levels.
- Hereditary Diseases: Look for a history of sickle cell disease or other genetic diseases.
- Chronic Illnesses: Examine history of cancer or other chronic illnesses that could affect the immune system or response to infections.
- Previous Symptoms of Malaria: Ask if the patient has ever had symptoms of malaria in the past.
Biological diagnosis of malaria
Malaria diagnosis relies on various methods, each offering specific advantages and considerations.
1- Complete Blood Count (CBC): Thrombocytopenia occurs in approximately 70% of patients, along with varying degrees of anemia observed in adults and up to 80% of children.
2- Urine Analysis: Proteinuria may be detected, indicating potentially nephrotic syndrome.
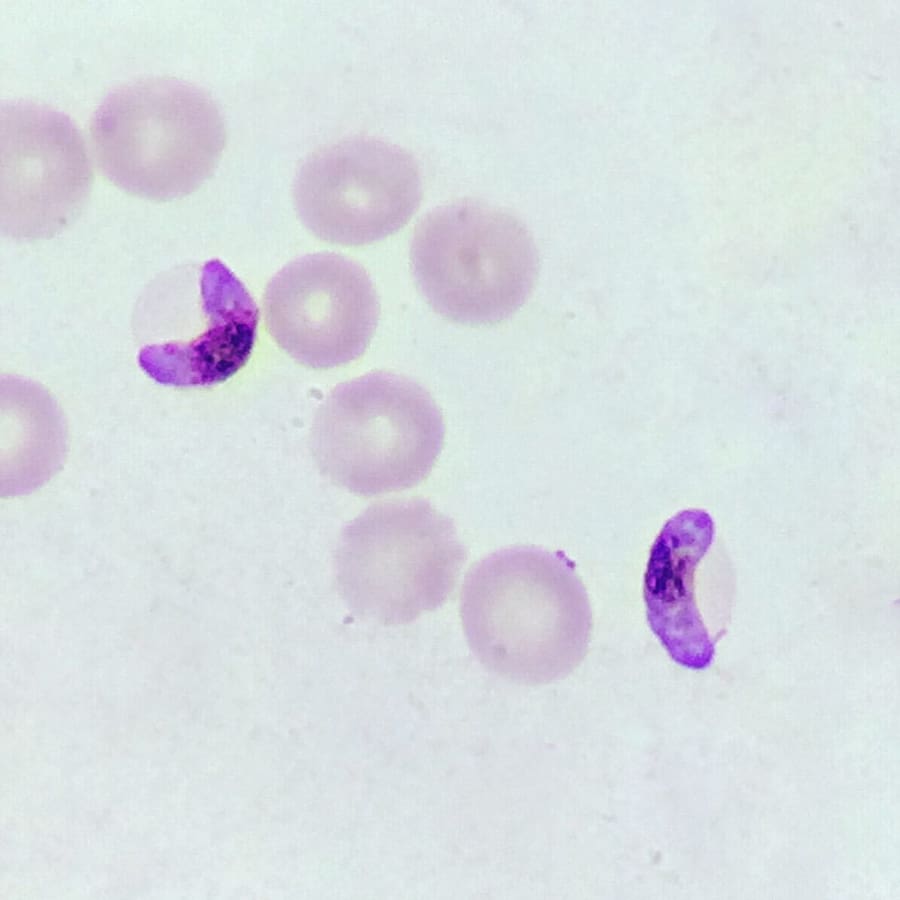
3- Blood Smear: Considered the gold standard for diagnosis, this method involves staining a blood smear with Giemsa stain and examining it microscopically. Using oil immersion for magnification ranging from 100 to 1000 times is imperative to detect low-level parasitemia or delicate ring forms.
a. Ring Stage Identification :
- P. falciparum: Appears as a purple dot with a thin ring.
- P. vivax: Purple spot with a deformed body.
- P. oval: Ring with a large purple dot.
- P. malariae: Purple spot with a thick body.
b. Identification of the Trophozoite Stage :
- P. falciparum: Larger spot surrounding a smaller one.
- P. vivax: Distorted circle containing an extended spot.
- P. oval: Oval circle containing a purple spot.
If the initial smear is negative, the possibility of intravascular sequestration of infected erythrocytes should be considered. In such cases, it is recommended to repeat the smear within 12 to 24 hours.
4- Rapid Diagnostic Test (RDT): Also called antigen test, this rapid method is used when examination of the blood smear is not possible. The RDT detects parasite antigens such as histidine-rich protein-2, lactate dehydrogenase, and aldolase, proving particularly useful in the diagnosis of P. falciparum infections.
5- Microhematocrit Centrifugation: This test isolates infected erythrocytes which bind to acridine in a collection tube, causing the parasite to fluoresce.
◉ Treatment / Prevention
The treatment of malaria includes several guidelines, including preventing mosquito bites and treating the disease itself.
A- Prevention of Mosquito Bites :
- Use of mosquito repellents on skin and clothing.
- Use of anti-mosquito coils and insecticide sprays.
B- Medical Treatment: with antimalarial drugs
- Chloroquine.
- Primaquine.
- Hydroxychloroquine.
- Artemisinin-based therapy.
◉ Conclusion
In conclusion, malaria remains a major public health challenge globally, requiring a multidimensional approach to its prevention, diagnosis and treatment.
Through increased awareness, targeted interventions and continued research, significant progress has been made in the fight against this devastating disease. However, concerted efforts and international collaboration are essential to achieve the ultimate goal of eliminating malaria and reducing its burden on the most vulnerable populations across the world.