Contents:
Laboratory Autoclave: Types and Principles
Definition
An autoclave is a steam sterilization device that uses moist heat in the form of saturated steam under pressure. This technique achieves temperatures above 100°C (up to 135-137°C), enabling the destruction of microorganisms including bacteria, viruses, fungi and their spores.
Steam sterilization offers several major advantages:
- Non-toxic to users and the environment
- Cost-effective compared to other sterilization methods
- Fast while ensuring excellent material penetration
Autoclaves are essential in laboratories, hospitals, pharmaceutical industries, and research centers. They can sterilize liquids, solids, and medical instruments of various sizes.

Autoclave Principle
Autoclave sterilization relies on four key parameters:
- Steam: Dry saturated steam ensures homogeneous heat transfer
- Pressure: Increases water temperature beyond normal boiling point
- Temperature: Typically 121°C (250°F) or 132°C (270°F)
- Time: Varies based on material type and packaging
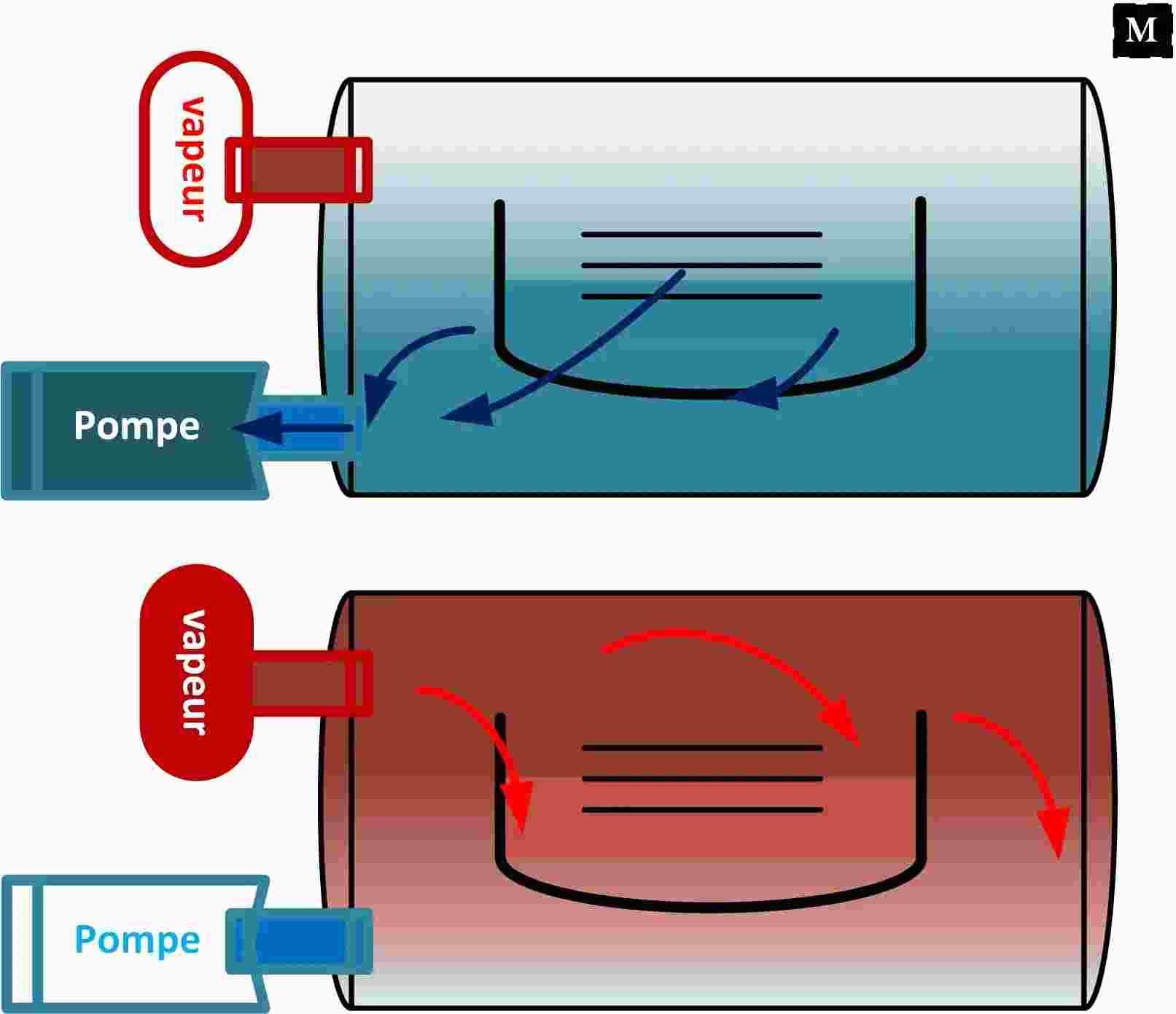
Two main methods are used:
- Gravity displacement: Naturally replaces air with steam - ideal for non-porous items
- Pre-vacuum: Air is completely removed first - better for porous/complex items

How Autoclaves Destroy Microorganisms
The primary mechanism relies on moist heat which causes:
- Coagulation of cellular proteins
- Irreversible denaturation of essential enzymes and microbial structures
Spores, the most resistant microbial forms, are also destroyed when exposed to appropriate temperatures and durations.
Compatible/Incompatible Materials
Compatible materials can withstand high temperatures and pressure without degradation. Incompatibilities typically involve chemical or plastic materials that may release toxic vapors or deform.
| Autoclave-Compatible | Autoclave-Incompatible |
|---|---|
|
|
Autoclave Types and Classes
When selecting an autoclave, there are three main types to consider:
Class B Autoclaves
Class B autoclaves are the most advanced models featuring:
- An external steam generator producing high-quality saturated steam quickly
- A vacuum drying system ensuring complete moisture removal post-sterilization
Typical applications:
- Hollow instruments (e.g., needles, cannulas)
- Porous instruments (like medical textiles)
- Packaged or unpackaged items
Class B autoclaves are essential in demanding medical environments such as hospitals, dental clinics, and research laboratories.
Class N Autoclaves
Class N autoclaves are simpler devices suitable only for:
- Solid, unpackaged instruments
- Simple objects not requiring deep steam penetration
Limitations:
- Cannot ensure uniform sterilization of hollow or porous instruments
- Lack effective drying systems, limiting use in applications requiring absolute sterility
Class S Autoclaves
Class S autoclaves offer an intermediate solution:
- Can sterilize simply packaged or multi-layer items and some complex instruments
- Equipped with a vacuum pump for better air removal than Class N, though less effective than Class B
Usage:
- Ideal for small facilities with moderate sterilization needs like medical offices or teaching labs
Factors Affecting Sterilization Efficiency
| Cleaning | Improper cleaning increases microbial load, protein residue, and salt concentration, reducing sterilization effectiveness. |
| Salt Residue | Residual salt decreases sterilization efficacy. |
| Restricted Flow | Sterilant must contact microorganisms. Device designs that prevent contact (e.g., tight turns) reduce effectiveness. |
| Protein Residue | Residual proteins decrease sterilization efficacy, though proper cleaning removes protein load. |
| Microbial Load | Higher initial contamination requires longer sterilization. |
| Overloading | Autoclaves shouldn't be overcrowded. Allow sufficient space for steam circulation. |
| Material Separation | Waste and clean items should be autoclaved separately. |
| Positioning | Items shouldn't touch chamber walls or top. |
| Cycle Selection | Incorrect cycle choice may damage autoclave, cause liquid overflow, or break containers. |
Conclusion
Autoclaves represent essential sterilization technology due to their effectiveness and versatility. By understanding their operating principles, different classes, and performance factors, users can optimize their operation for various laboratory, hospital, and industrial needs. Proper autoclave selection combined with rigorous protocols ensures impeccable sterility - crucial for infection prevention and user safety.