Content:
Howell Jolly bodies are small non-functional nuclear fragments that can be found, typically in splenic dysfunction, in the cytoplasm of red blood cells. This article focuses on the characteristics of Howell-Jolly bodies, examines the different detection methods and explores their clinical significance.
◉ What is the Howell-Jolly body?
Howell Jolly Bodies (HJBs) are a remnants of the cells nucleus that are normally removed by the spleen during the red blood cell maturation in the bone marrow. However, in some circumstances, they may persist.
While they are most commonly associated with splenectomy or hyposplenism (reduced spleen function), Howell-Jolly Bodies can also be seen in cases where there is an abnormal increase in the development of inclusions during erythropoiesis.
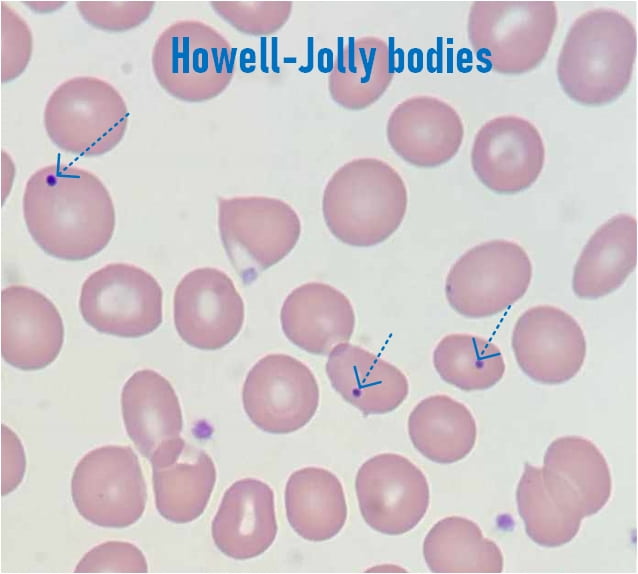
When observed under a microscope, these bodies appear as small, round, purple-staining inclusions. Its length is typically about 1 μm in diameter and can be seen in the peripheral blood smear using a light microscope.
They are named after the physician William Henry Howell and the hematologist Justin Marie Jolly, who first described them in the late 19th century.
Howell Jolly bodies
◉ Causes and Clinical significance of Howell-Jolly bodies
Since the spleen plays a vital role in removing abnormal or aged red blood cells, its absence or dysfunction results in the retention of Howell Jolly bodies within the circulating red blood cells. The most common causes of Howell Joll bodies are:
- Splenectomy: surgical removal of the spleen.
- Congenital asplenia: rare condition where an individual is born without a spleen.
- Heterotaxy syndrome: a rare birth defect that involves the spleen and other organs.
- Ivemark's syndrome: a congenital disorder characterized by multiple abnormalities, including absence, underdevelopment or malformation of the spleen
- Stormorken-Sjaastad-Langslet syndrome: a rare autosomal dominant disorder that affects the splenic function.
- Sickle cell diseas.
- Amyloidosis : may cause functional hyposplenism secondary to amyloid deposition in the white pulp and vessel walls.
- Alcoholism (can cause hyposplenism).
- Hemolytic anemia and megaloblastic anemia.
- Hereditary spherocytosis and myelodysplastic syndrome (MDS).
- Post-bone marrow transplantation : the function of the transplanted bone marrow may take time to fully recover, including the ability to produce normal red blood cells.
- Systemic lupus erythematosus : autoimmune disease that can cause splenic hypofunction or even asplenia.
- Folic acid deficiencies
- Vitamin B12 deficiencies
Interestingly, the presence of HJBs has also been reported in some severe cases of COVID-19, indicating the broad utility of these bodies as diagnostic indicators. In these cases, HJBs could be useful in distinguishing COVID-19 from bacterial pneumonia.
Note:
- In healthy individuals, red blood cells containing HJBs are found at a very low frequency.
- It is important to note that the presence of Howell Jolly bodies alone is not specific to a particular condition. Therefore, a thorough evaluation is necessary to determine the underlying cause.
◉ Detection of Howell-Jolly bodies
The Howell Jolly bodies detection can be performed using various laboratory methods, including:
◉ Howell-Jolly bodies on peripheral blood smears
To make a peripheral blood smear, a thin layer of blood is smeared on a glass slide, stained (Typically with May-Grunwald Giemsa stain (MGG)) and observed under a microscope.
Howell-Jolly bodies can be identified as small, round, dark structures inside red blood cells. They appear as distinct purple or blue-black dots against the lighter backdrop of the red blood cell. The size of Howell-Jolly bodies can vary, but are generally about 1-2 micrometers in diameter and typically one per RBC.

Howell-Jolly bodies on peripheral blood smears
◉ Automated blood cell analyzers
With technological advancements, automated blood cell analyzers have become widely used to detect Howell-Jolly Bodies. These analyzers use flow cytometry or laser-based technology to identify and quantify abnormal cells, including those containing HJBs. They provide a more objective and efficient approach to detecting these structures.
◉ Possible confusion
Howell-Jolly bodies can be confused with other similar structures or features observed in blood cells. Here are a few examples:
- Overlying platelets : but they do not have the “halo” that typically overlies platelets
- Basophilic stippling (punctate basophilia)
- Pappenheimer bodies : seen in certain types of anemia that are characterized by an increase in the storage of iron.
- Stain precipitate, Artifact.
- Heinz bodies : commonly associated with certain conditions that lead to oxidative stress or damage to the red blood cells.
◉ Importance of Howell-Jolly body detection
- Identifying Howell Jolly bodies is critical in patient treatment, especially with splenectomy patients.
- In individuals who have undergone splenectomy, the persistence of HJBs indicates a higher risk of developing certain complications, such as overwhelming post-splenectomy infection (OPSI).
- Monitoring the presence and quantity of these bodies in the blood might assist the effectiveness of vaccination protocols and guide decisions regarding prophylactic antibiotic therapy.
- Regular monitoring enables early detection of changes in the patient's splenic function and can aid in preventing potential complications.
- Additionally, HJBs in individuals without a history of splenectomy can prompt further investigation into suspected underlying medical issues.
- It serves as a red flag, emphasizing the need for a thorough to rule out any associated hematological or immunological problems.
◉ Conclusion
In conclusion, Howell Jolly bodies are small fragments of DNA found in red blood cells. Their detection and clinical significance have significant implications for patient management.
By its identification, healthcare professionals can monitor patients who have undergone splenectomy, guide vaccination and antibiotic prophylaxis strategies, and prompt further evaluation for underlying medical conditions. HJBs detection is crucial in optimizing patient care and ensuring timely interventions when necessary.